Record keeping for best practice
Published: 02/04/2015
High-quality clinical notes are essential for dental assessment and treatment planning. However, best practice has evolved, so records should also demonstrate the process by which a patient consented to their treatment option
Keeping well-documented patient records is an essential part of the health care system, including dental practices. High-quality clinical notes are essential to:
? Record details of patient assessment and to produce a treatment plan (Faculty of General Dental Practice (FGDP), 2007)
? Record treatment details
? Act as a legal record where dispute exists
? Facilitate practice administration and finance processes.
Patient records are increasingly important, due to an increase in litigation arising from patient complaints (Moyes, 2014). A complaint may more commonly be directed at a dentist or dental care professional (DCP) than a dental nurse, but it is often the dental nurse who creates the record.
Who can write patient notes?
The Scope of Practice publication from the General Dental Council (GDC), 2013a) states: ‘As a dental nurse, you can undertake the following if you are trained, competent and indemnified:
? Record dental charting and oral tissue assessment carried out by other registrants
? Keep full, accurate and contemporaneous patient records'.
However, the dentist working with you should check the records and sign or initial them. The time of the entry should also be recorded (FGDP, 2009).
Principle 4 of the GDC's (2013b)Standards for the Dental Team is: ‘Maintain and Protect Patient Information’. It advises that records must be:
? Contemporaneous
? Clear
? Accurate
? Legible and readily understood by others.
If it is necessary to add to records afterwards, or if it was found that an entry was made in error, do not delete the erroneous entry. Incorrect records should be struck through with a single line, then the additional entry added (along with the date and time) (FGDP, 2009). Falsifying records (for example, after a complaint is made) is considered dishonest and should not be attempted under any circumstances.
What should be included in patient records?
In addition to clinical notes and study models, the following comprise patients' records:
? Medical history forms
? Treatment plans (including fees)
? Laboratory instruction sheets
? Radiographs
? Clinical photographs
? Statements of conformity
? Forms signed to indicate consent given
? Copies of letters to and from patients
? Copies of referral letters.
If a patient makes a complaint against the practice or a member of staff, this information should not be included in the record card, but should be kept separately in the practice complaint file. This is so the patient is not disadvantaged or treated unfairly in the future when attending for treatment as a result of making the complaint.
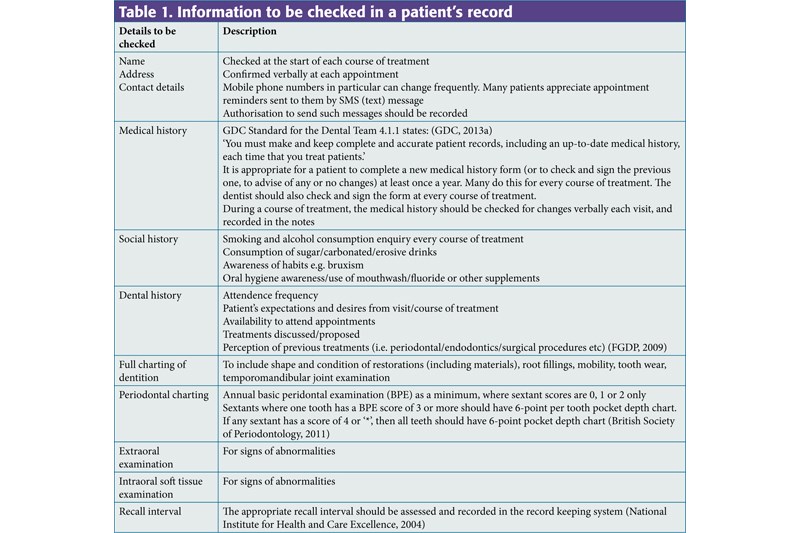
Following an examination, the information as outlined in Table 1 should be present and/or updated.
Table 1.
Information to be checked in a patient's record
| Details to be checked | Description |
|---|---|
| Name | Checked at the start of each course of treatment |
| Medical history | GDC Standard for the Dental Team 4.1.1 states: (GDC, 2013a) |
| Social history | Smoking and alcohol consumption enquiry every course of treatment |
| Dental history | Attendence frequency |
| Full charting of dentition | To include shape and condition of restorations (including materials), root fillings, mobility, tooth wear, temporomandibular joint examination |
| Periodontal charting | Annual basic peridontal examination (BPE) as a minimum, where sextant scores are 0, 1 or 2 only |
| Extraoral examination | For signs of abnormalities |
| Intraoral soft tissue examination | For signs of abnormalities |
| Recall interval | The appropriate recall interval should be assessed and recorded in the record keeping system (National Institute for Health and Care Excellence, 2004) |
Valid consent
Obtaining valid consent is Principle 3 of Standards for the Dental Team (GDC, 2013b). It requires the dental team to:
? Obtain valid consent before starting treatment, explaining all the relevant options and the possible costs
? Make sure that patients (or their representatives) understand the decisions they are being asked to make
? Make sure that the patient's consent remains valid at each stage of investigation or treatment (GDC, 2013b).
In addition, patients must be told everything they may wish to know, including:
? All the treatment options, risks and benefits given to a patient
? Which treatment option is considered most appropriate for the patient, and why
? The consequences, risks and benefits of the proposed treatment
? The likely prognosis for the recommended treatment
? The cost of the treatment
? The consequences of no treatment being carried out
? Whether the treatment is guaranteed (and how long for).
A complaint made against a dentist or DCP to the GDC can lead to an audit of record cards. If records are found to be incomplete or inadequate, further charges may be brought. These may relate to the clinical details, but lack of evidence of valid consent can be a significant issue.
The dental nurse is ideally placed to record discussions indicating valid consent was obtained; a dentist or DCP will often be gloved-up and unable to type. The dental nurse can create notes that are effectively contemporaneous and without risk of cross-infection breaches.
All treatment options, risks and benefits discussed should be recorded. Such discussions probably arise several times daily, so contemporaneous recording saves time, facilitates accuracy of records, and satisfies GDC requirements.
If a patient is referred for sedation or a general anaesthetic, the patient must sign a document confirming that they have been made aware of all treatment options, and all the risks.
Patients must be given enough time to consider information about treatment, and it must be given in a form they understand (i.e. avoiding technical jargon) (GDC, 2013b). It can be helpful to provide patients with printed ‘treatment information sheets' providing details of how procedures are performed, and the possible risks and benefits. Patients can sign these on their return to the surgery to indicate they have read them and consent to the treatment. A copy of the document can be given to the patient, and another retained in the patient's notes.
If changes need to be made to an agreed treatment plan, the changes must be discussed with the patient. Any changes, including any changes to the costs involved, must be agreed before treatment proceeds, and the consent should again be documented.
Radiographs
It must be possible to identify who justified and authorised the taking of every radiograph (National Radiological Protection Board, 2001). The Ionising Radiation Regulations 1999 and the Ionising Radiation (Medical Exposure) Regulations 2000 both state that the reason for taking the radiograph must be included, along with a report on findings from it (even if this is just ‘nothing abnormal detected’). A quality assurance system must exist, so each radiograph should be given a rating. A commonly used system is shown in
Table 2.
Radiograph quality assurance rating
| 1 | Excellent |
| 2 | Diagnostically acceptable |
| 3 | Unacceptable |
Treatment
When a patient attends for treatment, the planned procedure should be discussed. Verbal consent to continue must be obtained, and this should be recorded in the notes (GDC, 2013b).
The process by which a treatment came to be carried out should be recorded. An example is shown in
Table 3.
Example of a recorded treatment
| Step | Description | Notes might read |
|---|---|---|
| 1 | Date and time | 01.03.15 |
| 2 | On examination (o/e) (Followed by a description of what was found) | Patient indicated upper right quadrant o/e UR6 MO amalgam # |
| 3 | Periapical radiograph justified and authorised (J/A) by a dentist to check UR6 for apical pathology | P/A UR6 J/A (DD) to chk UR6 apex |
| 4 | Radiograph report on findings | P/A shows periapical radiolucency on UR6 palatal root and MO caries. All other teeth UR NAD. |
| 5 | Quality Assurance for radiographs | QA = 1 |
| 6 | Treatment options discussed: Extraction and possible implant needed/root canal treatment/advised if no treatment—pain likely to continue | Tx options disc: ELA (or XLA) and ? implant later/RCT/No Tx |
| 7 | Patient information sheets given with respect to extraction and root filling. Patient takes them away, signs them to indicate having read and understood them, copy taken and copy to patient: treatment option chosen recorded | Pt info given—pt considered—pt understands risks/would like ELA |
| 8 | Treatment recorded: date and time | 14.03.15 14:00 |
Where restorations are provided, the materials used and the tooth sufaces involved should be recorded. If the cavity is deep and there is an increased risk of the tooth becoming non-vital afterwards, the patient should be informed and this should be recorded in the records. The shades of any crowns or restorative materials should be recorded, along with any occlusal considerations.
Prosthetic treatments
Whether upper or lower (or both) jaws have impressions taken should be recorded, along with the materials used. It should also be recorded whether a ‘jaw registration’ was recorded (and using which material).
It should be recorded whether the patient (and clinician) were happy with the fit and aesthetics both at the “try in” and the “fitting”. A detailed laboratory prescription should be stored in the records along with the statement of conformity (FGDP, 2009). Tooth shades (and in the case of dentures, moulds) should also be recorded.
How long should records be kept?
Records should be kept for a maximum of 30 years (DH, 2009). As a minimum requirement they should be retained for 11 years (for children, they should be kept until the age of 25, or for 11 years, whichever is the later).
Referral letters
Whenever a patient is referred for secondary care, they should be offered a copy of all correspondence between clinicians (HM Government, 2000). A copy of the referral letter should also be kept in the patient's notes (FGDP, 2009).
sec-type="conclusions">Conclusion
In addition to recording clinical activity in a surgery, dental records must now demonstrate the process by which a patient provided valid consent to treatment. A dental nurse is ideally positioned to create a record of the conversations and clinical activity that precede consent being given (although this record must be verified and signed by the dentist).
Author: MA Healthcare